How Local AI Can Automate Insurance Tasks
Important: Consumer-Grade Hardware Focus
This guide focuses on consumer-grade GPUs and AI setups suitable for individuals and small teams. However, larger organizations with substantial budgets can deploy multi-GPU, TPU, or NPU clusters to run significantly more powerful local AI models that approach or match Claude AI-level intelligence. With enterprise-grade hardware infrastructure, local AI can deliver state-of-the-art performance while maintaining complete data privacy and control.
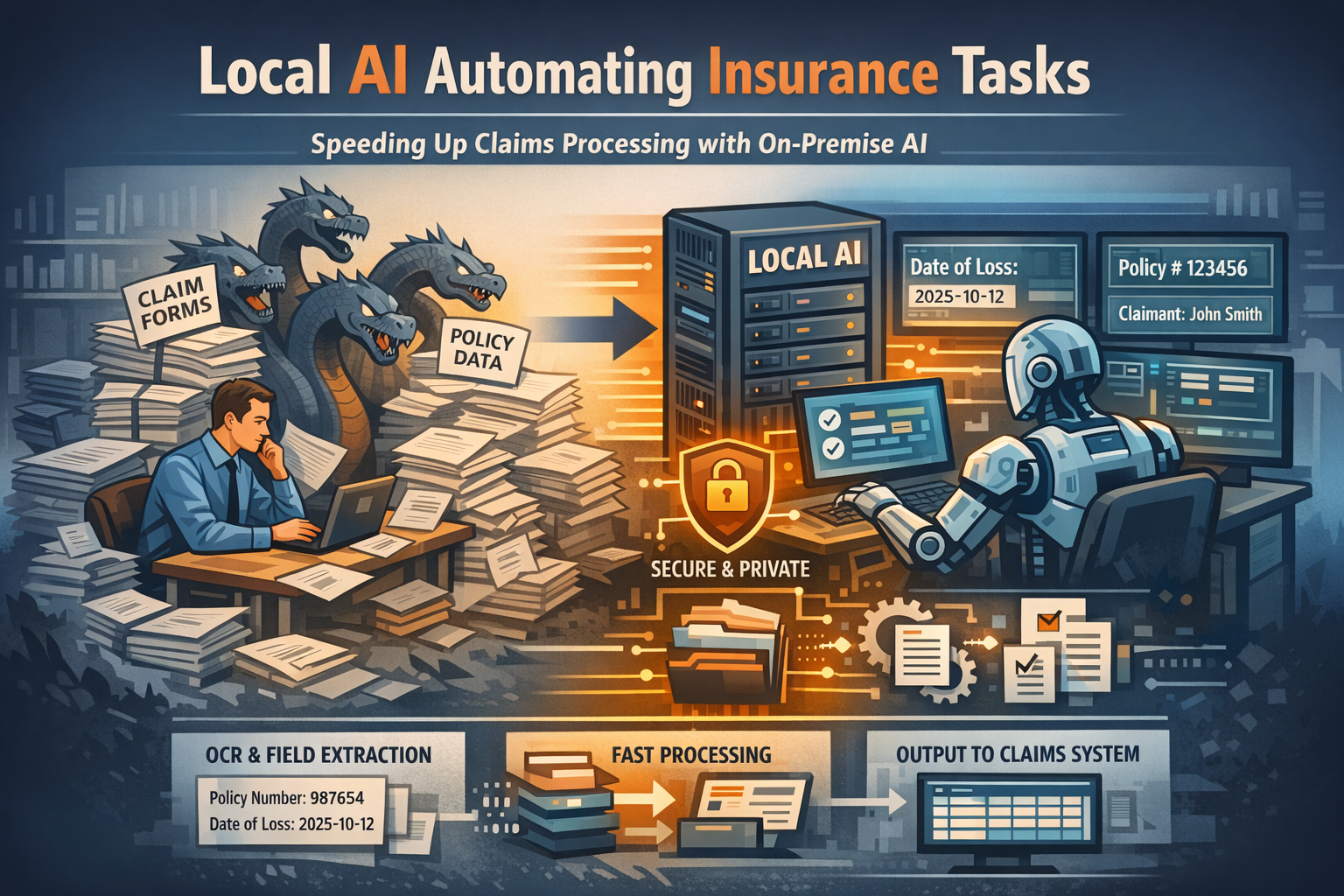
For insurance operations teams, processing claims and validating policies often feels like fighting a hydra: for every claim you settle, two more appear. The backlog isn't just about complex liability decisions or sensitive coverage disputes; it is frequently clogged with repetitive, rule-based data entry and document validation. Whether it's verifying thousands of policy renewals, extracting dates from scanned medical forms, or matching claim IDs to coverage limits, these "static" tasks consume hours of valuable adjuster and underwriter time.
These tasks share a common set of frustrations: they are high-volume, document-heavy, and unforgiving of human error. Yet, crucially, they require almost zero strategic judgment. You don't need years of underwriting experience to copy a policy number from a PDF to a database—you just need eyes and infinite patience.
This is exactly where Local AI thrives. Unlike general-purpose cloud chatbots that might try to "interpret" a policy clause or expose sensitive claimant data to third-party servers, local AI models (running privately on your own secure hardware) can be deployed as strict, deterministic engines. They don't "assess" risk; they simply process documents, extract fields, and format data with mechanical consistency.
Why These Tasks are "Static"
To understand where local AI fits, we must first define what makes an insurance task "static." A static task is one where the outcome is totally predictable and governed by fixed rules, regardless of the complexity of the document.
- Rule-Based: If a claim form lists "Date of Loss: 2025-10-12," that date is a fact, not an opinion. There is no ambiguity.
- Deterministic: The input (a scanned PDF, a handwritten form) should always yield the exact same output (a structured record, a validation flag).
- No Judgment Required: You aren't deciding if a claim is covered or how much to pay; you are simply recording what the claim data says.
Because these tasks rely on visual pattern recognition and strict data extraction rather than professional intuition, they are perfect candidates for automation.
Why Local AI is the Right Fit
You might wonder why you should use Local AI (like Llama 3, Mistral, or specialized GGUF models running on on-premise servers) instead of a cloud API or traditional OCR. For insurance, the advantages are specific and critical:
1. Privacy & Security: Insurance data contains highly sensitive PII and PHI (Protected Health Information). With local AI, medical records, policy details, and claimant identities never leave your secure infrastructure. You eliminate the risk of data leaks to public model providers.
2. Volume & Cost: Cloud AI APIs charge by the "token." When you are processing tens of thousands of pages of historical claims or policy documents, those costs skyrocket. Local AI runs for the fixed cost of your hardware and electricity.
3. Deterministic Control: By using specific parameters (like setting "temperature" to 0), local models can be forced to act as rigid data processors. This minimizes the risk of "hallucinations" or creative interpretations that are unacceptable in insurance.
4. Offline Capability: You can process sensitive data on air-gapped machines without any internet connection, ensuring a zero-trust environment for your most critical records.
What Local AI Actually Does (And What It Doesn't)
Local AI should be viewed as a tool for mechanical, deterministic actions. It assists the process but does not replace professional judgment.
Allowed Actions:
- Document Handling: Reading PDFs, handwritten forms, scanned images, and emails. It can "read" a crinkled accident report or a faxed medical form that traditional OCR might miss.
- Field Extraction: Pulling out specific, structured data points like Policy Number, Claim ID, Date of Loss, Insured Name, and Deductible Amount.
- Matching & Comparison: Comparing a claim's extracted data against a policy record to flag inconsistencies (e.g., "Claim date is outside policy period") or identifying duplicate claims.
- Classification: Categorizing documents by type (e.g., "Police Report," "Medical Invoice," "Estimate") or sorting incoming emails into "Urgent Claims" vs. "General Inquiries" based on keywords.
- Summarization (Non-Interpretive): Creating purely extractive summaries of claim descriptions or listing key facts (dates, locations, involved parties) from a narrative report.
- Formatting: Converting unstructured text (like an adjuster's field notes) into a structured JSON or CSV format ready for your claims management system.
What It Does NOT Do:
- Approve or deny claims.
- Assess liability or determine fault in an accident.
- Make underwriting decisions or price policies.
- Provide financial or legal advice to claimants.
Step-by-Step Workflow: Automating Claim Intake
Here is a practical, realistic workflow for using a local LLM to automate the initial intake and validation of high-volume claims documents.
1. Digitize and Prep
Gather your batch of incoming documents (PDFs, images). If they are scanned, use a local OCR tool or vision-enabled local model to convert them into raw text. High-quality text extraction is key to success.
2. Define the Schema
Create a strict prompt for the Local AI that defines exactly what you need. Do not ask it to "summarize the claim." Instead, command it:
"Extract the following fields from the document below into a strict JSON format: {"PolicyNumber": string, "DateOfLoss": "YYYY-MM-DD", "ClaimantName": string, "IncidentType": string}. If a field is missing, return null."
3. Batch Processing
Run a secure, local script (Python is standard) that iterates through your document folder. The script feeds each document's text into the local model with your prompt. Because it's local, you can process thousands of files overnight without API fees or data egress fees.
4. Validation Script
This is your safety net. Run a code-based validation script over the AI's JSON output.
- Does the "PolicyNumber" match the format of your active policies?
- Is "DateOfLoss" a valid date in the past?
- Is "ClaimantName" present?
Any record that fails these checks is flagged for manual review; valid records are passed to the next stage.
5. Formatting & Human Review
The valid data is converted into a standard format (CSV, XML) for your claims system. A claims processor opens this file, validates a random sample, and briefly reviews the flagged exceptions.
6. System Import
Once validated, the clean data—and the structured files—are imported directly into your Claims Management System (CMS). The manual data entry phase is effectively bypassed.
Realistic Example: The FNOL Bottleneck
Scenario: A regional auto insurer processes 500 First Notice of Loss (FNOL) emails and forms per week during storm season.
- Old Process: Three intake specialists spend 20 hours a week combined manually reading emails, typing data into the CMS, and assigning claims to adjusters.
- New Process with Local AI:
- A local batch process runs every hour, picking up new emails and PDF attachments.
- The AI successfully extracts and structures data for 460 of the 500 claims (92% automation).
- 40 claims are flagged as "unclear," "handwritten illegibly," or "missing policy number."
- The specialists spend just 2 hours reviewing the auto-processed batch and 1 hour handling the exceptions.
Result: The team saves 17 hours per week. Claims are assigned to adjusters hours faster, improving customer satisfaction. Specialists can focus on contacting distressed policyholders rather than typing data.
Limitations: When NOT to Use Local AI
It is critical to know your limits. Local AI is a powerful engine, but it acts without conscience or context. Do not use local AI for:
- Subjective Assessment: Determining if a driver was "negligent" based on a description. This is a legal and professional judgment.
- Coverage Disputes: Deciding if a specific, complex scenario falls under an exclusion clause.
- High-Value Decisions: Automatically approving payments or denying coverage. Automation stops at data entry and validation; the decision must remain human.
- Ambiguous Data: If a document is contradictory or unclear, the AI should be programmed to fail safely (flag it) rather than guess.
Key Takeaways
- Speed & Volume: Local AI excels at the "boring" work of reading, extracting, and formatting data from thousands of documents.
- Privacy Guaranteed: Processing sensitive claims data on your own hardware mitigates compliance and security risks.
- Assistance, Not Autopilot: The AI prepares the data for the human professional; it does not replace the underwriter or adjuster.
- Deterministic Output: Success relies on strict prompts, clear schemas, and rigid validation logic—not conversational "chat."
Local AI is best used as a deterministic assistant for high-volume, static insurance tasks where consistency, privacy, and volume matter more than judgment or reasoning.
Next Steps
Identify high-volume, repetitive tasks in your insurance operations:
- Are you manually entering claims data from PDFs or scanned forms?
- Do you spend hours extracting fields from FNOL emails or policy documents?
- Are you categorizing thousands of documents for claims processing?
- Do you need to validate policy numbers or coverage dates across large batches?
These are ideal candidates for local AI automation. Start with a small pilot project processing 100-200 claims to test accuracy and workflow integration before scaling to full production volumes.
For detailed implementation guides and model recommendations for insurance tasks, explore our technical documentation on local AI deployment in insurance environments.